Overcoming Barriers: Drug-Loaded Nanobubbles for Brain Cancer Therapy
Affecting and highly lethal, glioblastoma (GBM) is one of the most aggressive brain cancers, and it is uniquely resistant to standard therapies and a challenge for drug delivery across the blood–brain barrier (BBB). The BBB is a very selective barrier that protects the brain, but at the same time protects the brain from exposure to nearly all drug therapies for the GBM tumor site. To address this issue, as part of the NanoBio4Can Project, we have focused on a drug carrier known as nanobubbles (NB), which are novel, small, and impactful.
What Are Nanobubbles?
Nanobubbles are nanosized systems (1–300 nm) with a core-shell structure in which the core often contains gas, lipids, and drugs etc, and the shell is often, polymers. Their size and particular surface chemistry gives NBs prolonged circulation times after administration and effective drug encapsulation. In addition, unlike other nanoparticles, NBs can be activated by ultrasound to deliver drugs where they are needed more locally, and thus provide a more safe and targeted therapy.
How Nanobubbles are formulated for Glioblastoma
To develop drug-loaded nanobubbles, we used a high shear emulsification method. The bubbles encapsulate a clinically relevant chemotherapeutic agent. The goal is to optimize their particle size, stability, drug loading, and release kinetics necessary to ensure the bubbles are safe and effective.
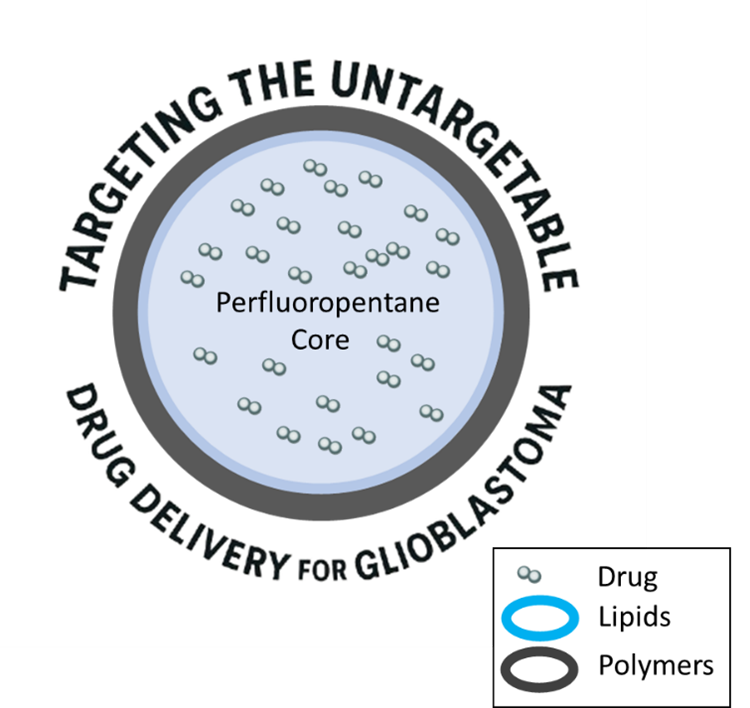
Sketch of Nanobubbles
Nanobubbles Characterization
To ensure reliability of the nanobubbles, we conducted extensive characterization of the nanobubbles:
- Dynamic light scattering (DLS): for size, polydispersity, and surface charge
- Electron microscopy (TEM and SEM): for shape and morphology
- In vitro drug release studies: drug release over 24 to 48 hours
- Stability studies: comparing nanobubble properties at cold storage conditions over three months
Why This Is Important
As a researcher in the NanoBio4Can Project, it is an incredible opportunity to develop stable, drug-loaded nanobubbles, which would be an important step for the treatment of brain cancer. In time, we may be able to safely cross the blood-brain barrier and directly treat GBM tumors with chemotherapeutic drugs. Furthermore, this combination may dramatically increase patient outcomes and reduce side effects compared with existing invasive or non-specific therapies.
To summarize, this work sets up a future where small bubbles may be responsible for big hopes in combating brain cancer.
Author: Shoeb Anwar Ansari, PhD
NanoBio4Can MSCA Co-Fund Fellow
Sabancı University Nanotechnology Research and Application Center (SUNUM)